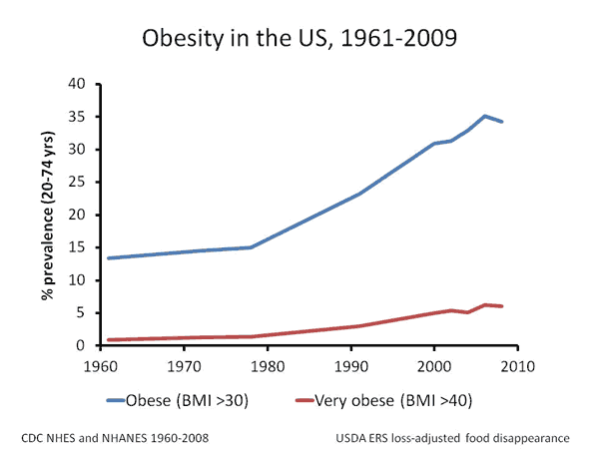
Duke University and CDC predict 42% of Americans will be obese by 2030. The impact on the nation's health (and economy) will be significant. Obesity is associated with many modern diseases such as diabetes, heart disease, metabolic syndrome, and sleep apnea. Other associations include migraine headaches, increased brain pressure (pseudotumor cerebri), rheumatoid arthritis, and inflammation of the brain's frontal lobes and hypothalamus.
Duke University and CDC predict 42% of Americans will be obese by 2030. The impact on the nation's health (and economy) will be significant. Obesity is associated with many modern diseases such as diabetes, heart disease, metabolic syndrome, and sleep apnea. Other associations include migraine headaches, increased brain pressure (pseudotumor cerebri), rheumatoid arthritis, and inflammation of the brain's frontal lobes and hypothalamus.
Obesity is measured using the Body Mass Index (BMI) and is calculated by dividing body weight by the square of the height. As noted by Medscape Neurology, BMI “is the most common means that clinicians use to define obesity.”
Central obesity, obesity of the abdomen, is also harmful to health. The extra adipose tissue collects below the skin (subcutaneous adipose tissue) and around the abdominal organs (visceral adipose tissue). While many of us grew up thinking extra fatty tissue was harmless, it is now understood that the adipose tissue of central obesity represents a “pathogenic tissue compartment” (a compartment of tissue that can make us sick).
In a study published in March 2012 issue of Age and Ageing, Dae Hyun Yoon MD, PhD and associates looked at the whether obesity, as measured by BMI, and central obesity affected brain function.
In 250 patients, 60 years of age or older, the amount abdominal fatty tissue (both visceral and subcutaneous) was measured on an abdominal CT scan and compared to the results on the MMSE-KC, a Korean diagnostic scale similar to the Mini-Mental State Examination that measures cognitive function. The researchers discovered that persons 60-70 years of age with a high BMI or high visceral obesity had significantly more difficulty with memory and thinking. According to Medscape Medical News:
After controlling for age, sex, education, hypertension, and diabetes, high BMI and being in the top tertile for visceral adipose tissue area were significantly associated with poor cognitive performance in those up to age 70 years.
Dr. Yoon explained:
Visceral adipose tissue is more metabolically active than subcutaneous adipose tissue and is thought to have a stronger influence on insulin resistance, among other things. It has long been considered as a pathogenic tissue compartment and this research shows a positive association between visceral adipose tissue area and low cognitive functioning. (emphasis added)
Contrary to popular belief, excess fat does not just sit there; it produces inflammatory substances that affect a variety of bodily functions. The extra fat impacts how the brain works; or, in this situation, doesn’t work.
Staffan Lindberg MD, PhD, writing in his medical textbook Food and Western Disease: Health and nutrition from an evolutionary perspective, notes that “overweight was extremely rare among hunter-gatherers.” As he shows, increasing evidence is pointing to the ancestral diet as the best model for reclaiming health.
To learn more about the ancestral human diet, consider these Ancestral Diet Resources. Also, take a look at the response in BMI and central obesity of these two dedicated Paleo advocates! (Unconquerable Dave and Diana)
Go Paleo to reduce and then get rid of obesity. Keep your brain sharp.
If you are on a special diet for health reasons, discuss the Paleo diet with your doctor before making changes. Also discuss with your doctor if you have high blood pressure or diabetes since your medications may need to be lowered. Also, if you are on Coumadin or have hemochromatosis, discuss this diet with your doctor before you start.
 Monday, December 23, 2013 at 07:50AM
Monday, December 23, 2013 at 07:50AM  Image: Mosborne01Is a child’s weight or their aerobic fitness the better predictor of academic performance? Researchers of the Partnership for Healthy Lincoln in Nebraska studied this question in fourth- to eighth-grade students and published their findings in the August 2013 Journal of Pediatrics.
Image: Mosborne01Is a child’s weight or their aerobic fitness the better predictor of academic performance? Researchers of the Partnership for Healthy Lincoln in Nebraska studied this question in fourth- to eighth-grade students and published their findings in the August 2013 Journal of Pediatrics.