Guest Post by Gerard Guillory, M.D.
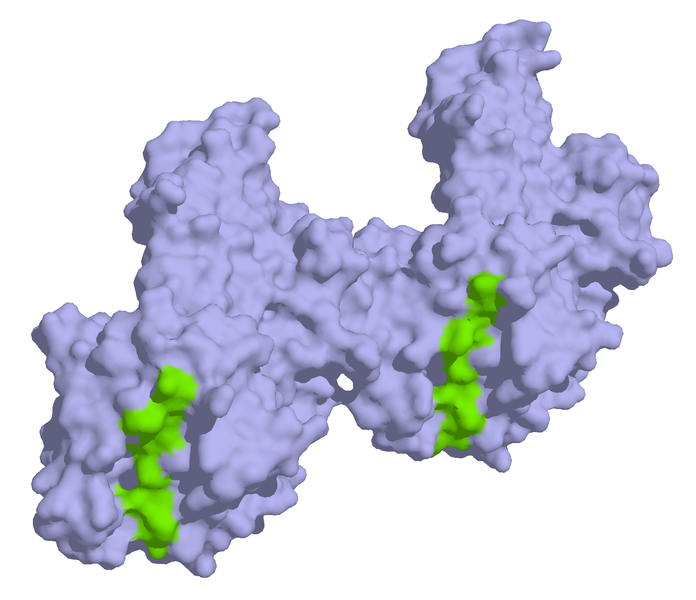
 Approximately 1% of persons in the US have celiac disease, an immune reaction to the gluten protein in wheat (above), barely, rye and sometimes oats. Many more may sensitive to this foreign protein.Gluten sensitivity is more common than medical experts once believed, affecting perhaps as much as 1 percent of the U.S. population. The symptoms of this condition, also referred to as celiac disease, can be widely varied and highly unpleasant. The good news is that celiac disease can be detected through a simple blood test and effectively managed through changes in diet.
Approximately 1% of persons in the US have celiac disease, an immune reaction to the gluten protein in wheat (above), barely, rye and sometimes oats. Many more may sensitive to this foreign protein.Gluten sensitivity is more common than medical experts once believed, affecting perhaps as much as 1 percent of the U.S. population. The symptoms of this condition, also referred to as celiac disease, can be widely varied and highly unpleasant. The good news is that celiac disease can be detected through a simple blood test and effectively managed through changes in diet.
Gluten is a protein found in wheat, barley and rye and food products such as breads and pastas that are derived from these grains. Gluten also is sometimes found in oats, which frequently are contaminated with gluten during processing and, as a result, also contain the protein.
In some people, the body’s immune system is triggered by the presence of gluten, causing a variety of problems. In children, these can include failure to thrive and short stature. Many gluten-sensitive adults experience chronic gastrointestinal problems, including diarrhea, flatulence and weight loss. Recent studies have indicated that many adults who are gluten-sensitive experience non-gastrointestinal problems as well, including iron-deficiency anemia and decreased bone density.
I became interested in gluten sensitivity in 1989, when I wrote my first book on irritable bowel syndrome (IBS). I had included a chapter on the so-called elimination diet. In those days, we didn’t have effective tests for many food allergies, so we recommended that patients eliminate various foods from their diet and then resume consumption of these, one by one. This would help identify the cause of IBS symptoms.
Through this method, we found that when some patients eliminated gluten from their diets, not only did IBS symptoms disappear, but so did other problems such as rheumatism, allergies and skin disorders.
Recent studies suggest that this isn’t a coincidence; in fact, there appears to be a direct link between gluten and auto-immune disorders. If you have an auto-immune disorder such as rheumatism, I recommend that you ask your physician about gluten sensitivity and consider getting a blood test. You also should consider testing if you are experiencing unexplained gastrointestinal problems such as chronic diarrhea or weight loss. Testing should be done before you attempt to eliminate gluten from your diet, so that the lab can determine whether gluten is triggering an immunological response.
If you test positive for celiac disease, your physician is likely to recommend that you work with a dietician to develop a gluten-free diet. Many people also join a support group, which helps them stay with the diet. Growing numbers of grocery stores and natural-foods stores sell gluten-free products, so the difficulties associated with the diet are perhaps not as onerous as they once were.
Gerard L. Guillory, M.D., is board-certified in internal medicine and has been practicing in Aurora, Colo., since July 1985. As an assistant clinical professor of medicine at the University of Colorado Health Sciences Center, Dr. Guillory is actively involved in teaching medical students, resident physicians, and nurse practitioner students. He has lectured extensively on the role of nutrition and disease. Over the years, he has fostered an interest in patient education and has authored three books on digestive troubles.
Originally posted at The Care Group, update Feb 7, 2011
 Saturday, November 2, 2013 at 08:10AM
Saturday, November 2, 2013 at 08:10AM  Celiac disease,
Celiac disease,  CrossFit,
CrossFit,  Paleo diet in
Paleo diet in  Success Stories
Success Stories